Medical Research Safety: How Funding Cuts Affect Patients
Medical research safety is paramount in protecting the integrity of clinical trials and the well-being of participants. As federal funding cuts threaten vital oversight mechanisms, it becomes crucial to understand the impact on patient safety and research ethics. Oversight bodies, such as Institutional Review Boards (IRBs), are integral in reviewing and approving studies to ensure compliance with health regulations, thereby safeguarding participants. Without the necessary resources, the research governance landscape faces significant challenges, potentially undermining the rights of those involved in medical studies. In a time when innovation sparks hope for breakthroughs in treatment, fostering a culture of safety within medical research cannot afford to be compromised.
The realm of medical research safety encompasses a wide variety of elements essential to the ethical conduct of clinical trials. This aspect of research governance involves ensuring that study participants are protected and their rights upheld throughout the research process. With an emphasis on patient welfare, entities tasked with clinical trial oversight play a critical role in maintaining ethical standards and overseeing the research protocols. In light of recent discussions surrounding IRB funding and associated budget cuts, the operational capacity of these ethical review boards may be severely affected. Ultimately, the focus remains on safeguarding volunteers and patients who contribute their time and health to advance our medical knowledge.
Impact of Funding Cuts on Medical Research Oversight
The recent halt in over $2 billion in federal research funding has starkly revealed the essential role that financial resources play in ensuring rigorous oversight of medical research. When funding is cut, institutions face significant operational disruptions, particularly in systems like the SMART Institutional Review Board (IRB) that are crucial for patient safety. This interruption can directly affect the applications and studies that rely on adequate oversight from resource personnel who understand the nuances of medical ethics and research compliance.
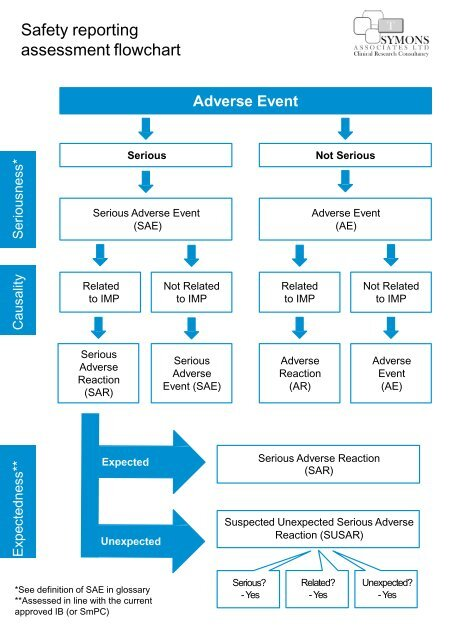
Moreover, delays in multi-site studies can lead to frustrated researchers, disjointed collaborations, and disillusioned participants. The multifaceted governance of clinical trials typically includes oversight mechanisms designed to mitigate risks, but with reduced funding, the capacity for thorough review diminishes. The consequences can ripple through the community as unmet needs for patient safety and ethical standards in research become prevalent, potentially undermining public trust in clinical trials.
The risks amplifying from these funding cuts are particularly concerning as they jeopardize not just research progress, but also the very safety of patients involved in these trials. Without adequate resources to conduct necessary reviews, monitoring, and adjustments to protocols, the likelihood of adverse events may increase, raising ethical questions regarding informed consent and risk management.
Ultimately, the suspension of funding can stifle innovation and put patient well-being at risk, pointing to a dire need for comprehensive funding that ensures oversight systems equipped to protect individuals participating in vital health research.
The Essential Role of Institutional Review Boards (IRBs)
Institutional Review Boards (IRBs) serve as a bedrock of the medical research landscape, ensuring that studies involving human participants adhere to rigorous ethical standards and regulatory compliance. These boards are responsible for evaluating research proposals to confirm that they align with established ethical principles, assess risk mitigation strategies, and safeguard the welfare of research participants. Through ample review processes, IRBs foster environments where patient rights are prioritized, directly contributing to patient safety in clinical trials.
However, the functionality of IRBs is threatened during periods of funding austerity, as resource limitations restrict their ability to conduct comprehensive oversight. This can result in increasing gaps in patient protection and oversight, compromising the integrity of research practices. Proper IRB functioning includes not just initial review but ongoing monitoring throughout the research lifecycle to ensure participant safety and adherence to ethical mandates.
When funding cuts are imposed, many IRBs may struggle to maintain staffing levels and support necessary training, impacting their capacity to fulfill their roles effectively. Historical instances where oversight failed serve as reminders of the importance of sustained support for IRBs, demonstrating the necessity of governance structures to protect research participants from harm. With the implications of funding cuts echoing through medical research, maintaining adequately financed IRB oversight is indispensable for keeping studies ethical and safe.
In view of these challenges, advocacy for sustained financial support for IRBs becomes critical. Researchers, institutions, and the public must recognize the value of IRB governance in facilitating ethically founded studies that prioritize not only scientific advancement but also the protection of individuals and communities engaged in research.
Navigating Research Ethics in the Face of Budget Cuts
Research ethics represent a core element of medical studies involving human participants, providing the necessary framework to ensure respectful and dignified treatment of individuals involved in these trials. Cutting research funding can severely complicate the practical application of research ethics, as financial resources are pivotal in fostering comprehensive oversight and accountability mechanisms. Inadequate funding can impede the essential training provided to investigators and research team members, increasing the risk of ethical breaches and compromising patient safety.
Moreover, the Principles of Good Clinical Practice dictate that ethical considerations must permeate every aspect of research, from design to implementation. A reduction in resources hampers the ability to conduct thorough ethical reviews and the necessary monitoring of ongoing trials, raising concerns about the adequacy of informed consent processes and the overall safety of participants. Ethicists argue that financial commitment is intrinsically linked to the integrity of the research process, emphasizing that protection of research participants should never be considered a lower priority.
While institutional regulations and public trust are integral components of the research ecosystem, they require backing from robust funding sources to thrive. The push for comprehensive and uninterrupted funding reflects the urgent need to safeguard ethical research practices amid changing political landscapes, underscoring how intertwined research funding and research ethics are for the promotion of patient safety.
As the landscape of medical research evolves—especially in light of budget constraints—it is essential to reinforce the ethical foundations that govern research practices. Supporting the ethical infrastructure not only boosts individual protection but also advances trust in medical research as a whole.
Collaborative Research and Patient Safety: Balancing Acts
Collaborative research initiatives often span multiple institutions and disciplines, offering potentially groundbreaking advancements in healthcare. However, the benefits of this teamwork can be undermined by funding cuts, which impede robust patient safety mechanisms that should accompany such collaborative efforts. When varied stakeholders collaborate on a clinical trial, the need for cohesive governance is essential to protect study participants and ensure adherence to ethical research standards.
Conflicting priorities among partners and the lack of adequate resources can foster an environment where ethical oversight becomes an afterthought rather than a priority. Collaborative agreements typically emphasize shared responsibilities for patient safety and compliance with research ethics, but these objectives can weaken without proper financial backing.
Thus, ensuring patient safety within collaborative research frameworks requires persevering support for oversight mechanisms that streamline compliance and risk assessment across diverse study sites. The advantage of collaboration lies in comprehensive knowledge sharing, yet this potential is only realized when the necessary infrastructure—such as centralized IRB reviews and oversight mechanisms—is adequately funded.
In conclusion, as we navigate the complexities of collaborative research, it becomes clear that safeguarding patient safety hinges on our ability to secure sustained financial investment. The call for increased funding reaches beyond advancement—it is a vital necessity to balance innovation and protection in clinical research.
Strategies to Mitigate Impacts of Funding Reductions
In light of current funding cuts to medical research, proactive strategies to mitigate adverse impacts on patient safety and ethical oversight are essential. Institutions can explore alternative funding sources such as partnerships with private industry, crowdsourcing for patient advocacy groups, and seeking collaborations with non-profit organizations. Leveraging diverse funding avenues not only increases resources available for research but also invites accountability from various stakeholders, reinforcing the commitment to patient welfare.
Additionally, adopting innovative technologies can also enhance research oversight and patient safety in an era of budget constraints. Digital platforms for tracking compliance, streamlined consent processes, and remote monitoring for trial participants can reduce costs while maintaining rigorous standards. Emphasizing efficiency enables research facilities to navigate funding challenges while still prioritizing patient protection and adherence to ethical principles.
Furthermore, involving patients and communities in the research process can also foster heightened transparency and enhance participant engagement with the research community. When patients feel a sense of ownership and understanding of the research, they are more likely to advocate for their safety, ultimately leading to a more ethically sound research environment.
Exploring these strategies as part of a broader effort to combat funding shortages can bolster the integrity and safety of medical research initiatives while simultaneously renewing public trust in the scientific process.
Historical Context: Lessons Learned in Medical Research Ethics
The history of medical research has profoundly shaped our understanding of ethical practice and respect for patient rights. Past atrocities, such as the Tuskegee Syphilis Study and the unethical hepatitis studies of vulnerable populations, serve as stark reminders of the consequential need for oversight measures to safeguard human subjects. Each incident paved the way for enhanced scrutiny and regulations that govern contemporary clinical trials, reflecting society’s evolving recognition of research ethics.
However, even with established guidelines in place, the effects of funding cuts pose a tangible risk of reverting to practices that could jeopardize patient safety. Constant vigilance regarding ethical practices, ongoing training for research professionals, and institutional commitment to ethical conduct are fundamental components to prevent history from repeating itself.
Current discussions surrounding medical research governance must prioritize historical lessons while advocating for sustained funding to honor the commitments made to protect participants. As we strive toward innovative developments in healthcare, embedding historical understanding within the fabric of research practices can help prevent ethical oversights and enhance research integrity.
In conclusion, the intersection of history and current challenges in medical research ethics speaks to the critical importance of investing in the robust oversight systems that enhance both patient safety and trust in clinical trials.
The Role of Advocacy in Safeguarding Research Funding
In times of funding crises, the role of advocacy organizations and patient advocacy groups becomes increasingly vital. These entities serve as champions for the rights of research participants and can raise awareness about the direct implications of financial cuts on patient safety and ethical research practices. By mobilizing stakeholders and the public, advocacy groups can drive conversations that emphasize the necessity for governmental and institutional commitment to sustain funding for medical research.
Additionally, advocacy can extend beyond addressing immediate funding needs. By calling attention to the importance of medical research financial investment, advocacy organizations can pave the way for long-term solutions that emphasize the ongoing need for patient safety, ethical oversight, and collaborative governance. Efforts to maintain open dialogues with legislators and funding bodies regarding the value of medical research can assist in building a resilient ecosystem supporting both research advancement and patient protection.
In summary, the power of advocacy lies in its ability to spotlight critical issues and mobilize action. By becoming proactive participants in the discourse around funding and governance, advocates can bolster necessary support to ensure that patient safety remains paramount in the face of financial uncertainty.
Frequently Asked Questions
What is medical research safety and why is it important?
Medical research safety refers to the practices and protocols established to ensure the protection of participants involved in clinical trials and studies. Ensuring medical research safety is vital to protect the rights and welfare of research participants, which fosters public trust and supports the integrity of the research process.
How do institutional review boards (IRBs) enhance patient safety in medical research?
Institutional review boards (IRBs) play a critical role in enhancing patient safety in medical research by reviewing study protocols, assessing risks, and ensuring that informed consent processes are in place. They act as an ethical oversight mechanism, striving to protect the rights and safety of individuals participating in clinical trials.
What are the consequences of funding cuts on patient safety in medical research?
Funding cuts can severely disrupt medical research safety by limiting the operational capabilities of IRBs and halting ongoing studies. This can lead to inadequate oversight, increased risks for participants, and a loss of public trust in the research community, ultimately affecting the safety and efficacy of new treatments.
How does research ethics relate to medical research safety?
Research ethics encompasses the principles and guidelines that govern the conduct of medical research to ensure safety, dignity, and rights of participants. It is intrinsically linked to medical research safety, as ethical oversight ensures that participants are treated fairly, informed consent is obtained, and their welfare is prioritized throughout the research process.
What role does clinical trial oversight play in ensuring patient safety?
Clinical trial oversight involves continuous monitoring and evaluation of studies to ensure compliance with safety protocols and ethical standards. Effective oversight safeguards patient safety by ensuring that any adverse events are promptly addressed, maintaining the integrity of the research process, and enhancing overall public trust.
How do federal funding cuts impact medical research governance?
Federal funding cuts can diminish the capacity for medical research governance by reducing resources for vital oversight bodies like IRBs. This can result in compromised patient safety, as essential governance practices may not be adequately implemented, and the integrity of research studies may be jeopardized.
What systems are in place to address patient safety in multi-site medical research?
The SMART IRB system is designed to streamline and centralize review processes for multi-site medical research. By facilitating oversight and ensuring consistent application of safety protocols across multiple institutions, this system significantly enhances patient safety in collaborative research endeavors.
Why are patient safety considerations critical in research involving vulnerable populations?
Patient safety considerations are especially critical in research involving vulnerable populations to protect them from exploitation and harm. Special ethical protections must be in place to ensure that these groups fully understand the risks and benefits, securing their rights and safety throughout the research process.
What historical events highlight the importance of medical research safety?
Historical events such as the Tuskegee Syphilis Study and unethical medical experiments during World War II emphasize the critical need for stringent medical research safety protocols. These incidents underline the importance of oversight and ethics to prevent harm and to maintain public trust in scientific research.
How can researchers minimize risks to patients in medical studies?
Researchers can minimize risks to patients in medical studies by implementing thorough risk assessments, ensuring ethical review by IRBs, obtaining informed consent, and maintaining transparent communication with participants about the study’s objectives, risks, and potential benefits.
| Key Points | Details |
|---|---|
| Funding Freeze Impact | The Trump administration’s freeze of over $2 billion in federal research grants has disrupted medical research safety efforts. |
| SMART IRB Role | SMART IRB facilitates oversight of multi-site medical research, crucial for patient safety and rights. |
| IRB Function | Institutional Review Boards (IRBs) ensure compliance with laws and safeguard participant welfare in research. |
| Historical Importance | Historically significant events unveiled the necessity of IRBs for ethical oversight in clinical trials. |
| Consequences of Funding Cuts | Halting of studies and inability to add new clinical sites negatively impacts participant safety and research integrity. |
| Support from Harvard Medical School | Despite funding cuts, ongoing support aims to uphold collaborative research and safeguard public health. |
Summary
Medical research safety is significantly hindered by funding cuts, as they disrupt essential oversight mechanisms like the SMART IRB. The freeze of over $2 billion in federal grants has caused critical delays and halted studies, endangering the welfare of research participants. Institutional Review Boards (IRBs) are vital in protecting participants’ rights and ensuring ethical research practices. The impact of these funding cuts can undermine public trust and safety in medical research, emphasizing the need for systematic support and funding to maintain safe and ethical research environments.
You may also like
Archives
Calendar
| M | T | W | T | F | S | S |
|---|---|---|---|---|---|---|
| 1 | ||||||
| 2 | 3 | 4 | 5 | 6 | 7 | 8 |
| 9 | 10 | 11 | 12 | 13 | 14 | 15 |
| 16 | 17 | 18 | 19 | 20 | 21 | 22 |
| 23 | 24 | 25 | 26 | 27 | 28 | |